Haglund’s Bony Protruberance Causing Bursitis and Achilles Tendon Pain
A bony growth that appears at the back of the heel bone can occur. This growth is called an exostosis (a benign cartilaginous growth) and is known as Haglund’s Deformity. This bony prominence can rub against the overlying Achilles tendon and causes pain in the tendon. A small sac (called bursa) that lies between the bone and the Achilles tendon usually becomes inflamed and swollen. This is called retrocalcaneal bursitis. The syndrome is caused by repetitive impingement of the bursa between the ventral aspect (front) of the Achilles tendon and the posterosuperior calcaneal prominence (heel spur). Typically, patients have pain when they start to walk after a period of rest.
Signs & Symptoms
Haglund’s deformity can occur in one or both feet. The signs and symptoms include:
-
A noticeable bump on the back of heel
-
Pain in the area where the Achilles tendon attaches to the heel.
-
Swelling in the back of the heel.
-
Redness near the inflamed tissue
Haglund’s Disease is characterized by pain and tenderness at the posterolateral aspect of the calcaneus (heel bone) where a calcaneal prominence (heel bone spur) can be palpated. This entity also is known as ‘‘pump-bump.’’ A distinction between Haglund’s disease and other pathologic conditions, such as a superficial Achilles bursitis (inflammation), must be made. Haglund’s syndrome involves a painful swelling of an inflamed retrocalcaneal bursa (a small fluid filled sac located at the back of the heel), sometimes combined with the degeneration of the fibers of the Achilles tendon directly at its insertion into the heel bone (insertional tendinopathy of the Achilles tendon).
Cause
High arches (pes cavus) can contribute to Haglund’s deformity. The Achilles tendon attaches to the back of the heel bone, and in a person with high arches, the heel bone is tilted backward into the Achilles tendon. This causes the uppermost portion of the back of the heel bone to rub against the tendon. Eventually, due to this constant irritation, a bony protrusion develops and the bursa becomes inflamed. It is the inflamed bursa that produces the redness and swelling associated with Haglund’s deformity. A tight Achilles tendon can also play a role in Haglund’s deformity, causing pain by compressing the tender and inflamed bursa. In contrast, a tendon that is more flexible results in less pressure against the painful bursa. Another possible contributor to Haglund’s deformity is a tendency to walk on the outside of the heel (varus heel). This tendency, which produces wear on the outer edge of the sole of the shoe, causes the heel to rotate inward, resulting in a grinding of the heel bone against the tendon. The tendon protects itself by forming a bursa, which eventually becomes inflamed and tender.
Diagnosis
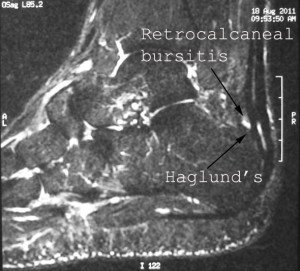
MRI of Haglund’s with Retrocalcaneal Bursitis
There is usually pain in the Achilles tendon insertion into the calcaneus (heel bone) posteriorly (behind). The Achilles tendon can be thickened (swollen) and tight. There is pain in the retrocalcaneal bursa (see the 1st picture in this article). A check for high arch of the foot as well as the heel from the back with the patient standing is done to make sure there is no heel varus (the heel points inwards when standing). These physical signs usually point to poorer results with treatment. An X-ray of the heel can be done to look for any Haglund’s exostosis or deformity. An MRI scan can be done. This is useful to diagnose Achilles tendinosis (which is related to the Haglund’s bump), swelling of the sac between the Haglund’s bump and Achilles tendon (retrocalcaneal bursitis).
Haglund’s Deformity and Heel Spur Treatment
Non-Surgical Treatment
A Non-surgical treatment of heel spur and Haglund’s deformity is aimed by a foot and ankle specialist in Singapore at reducing the inflammation of the bursa. While these approaches can resolve the bursitis, they will not shrink the bony protrusion. Non-surgical treatment can include one or more of the following:
- Medication – Anti-inflammatory medications may help reduce the pain and inflammation. Some patients also find that a topical pain reliever, which is applied directly to the inflamed area, is beneficial.
- Ice – To reduce swelling, apply a bag of ice over a thin towel to the affected area for 20 minutes of each waking hour. Do not put ice directly against the skin.
- Exercises – Stretching exercises help relieve tension from the Achilles tendon. These exercises are especially important for the patient who has a tight heel cord.
- Heel lifts – Patients with high arches may find that heel lifts placed inside the shoe decrease the pressure on the heel.
- Heel pads – Placing pads inside the shoe cushions the heel and may help reduce irritation when walking.
- Shoe modification – Wearing shoes that are backless or have soft backs will avoid or minimize irritation.
- Physical therapy – Inflammation is sometimes reduced with certain forms of physical therapy, such as ultrasound therapy.
- Orthotic devices – These custom arch supports are helpful because they control the motion in the foot, which can aggravate symptoms.
- Immobilization – In some cases, casting may be necessary to reduce symptoms.
Surgical Treatment
If non-surgical treatment fails to provide adequate pain relief, surgery may be needed. Operative heel spur treatment in Singapore consists of removal of the inflamed bursa and resection of the bony prominence. This can be done by the traditional open surgical technique with a 3cm to 4cm scar or a minimally invasive endoscopic technique using 2 small stab incisions. A minimally invasive procedure to remove Haglund’s bony prominence is called Endoscopic Calcaneoplasty. Endoscopic Calcaneoplasty The operation is performed under general or regional anesthesia with the patient in a prone position.

The patient is in a prone position. The opposite leg is held away from the surgical field.
Fluoroscope (x-rays) is used to localise the position of the Haglund’s exostosis.

Fluroscopic Localisation of Haglund’s
A small vertical incision is made through the skin at the level of the superior aspect of the calcaneus. The retrocalcaneal space is penetrated by a blunt trocar. A 4.5-mm arthroscope is introduced into the retrocalcaneal space. Under direct vision a spinal needle is introduced just medial to the Achilles tendon, again at the level of the superior aspect of the calcaneus, to locate the medial portal. After making a vertical stab incision, the 3.5-mm full radius resector is placed and visualized by the arthroscope. The inflamed retrocalcaneal bursa is removed to provide a better view. The superior surface of the calcaneus is visualized, and its fibrous layer and periosteum is stripped off using a radiofrequency wand.
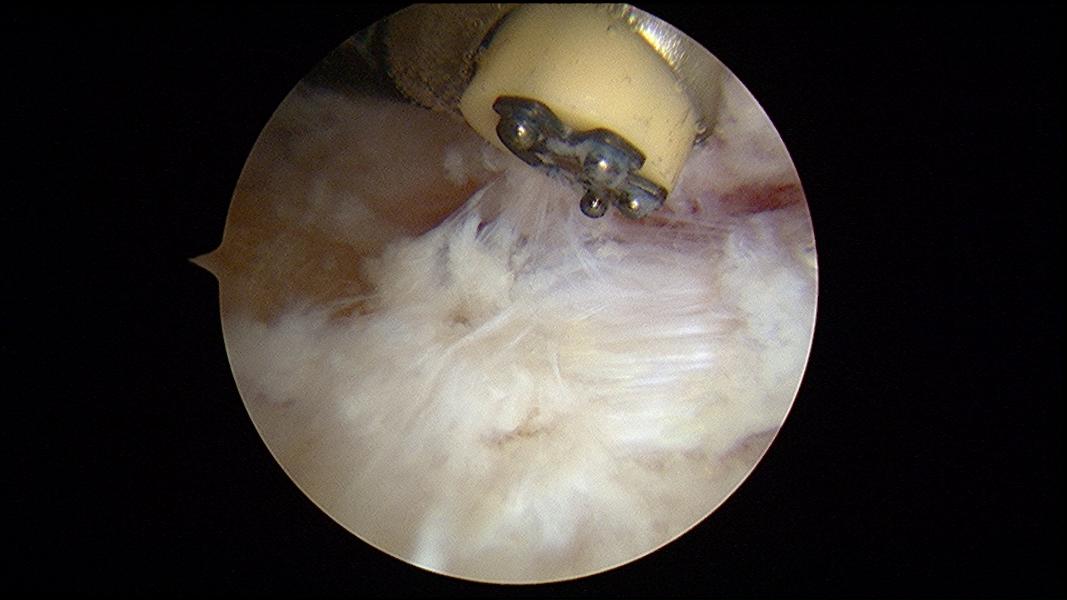
Using radiofrequency wand to clear soft tissue
The Haglund’s exostosis is exposed.

Haglund’s exostosis with foot in neutral position
When the foot is brought into full dorsiflexion, the impingement site is determined.

Haglund’s exostosis impinging the Achilles tendon with foot in dorsiflexion
A 4.0mm hooded arthroscopic burr is used to remove the Haglund’s exostosis. All of the time the opening of the burr is facing the bone. The foot is placed in full plantarflexion and the posterior superior bone rim can be removed.

Burring away the Haglund’s exostosis
Upon completion of the procedure, the exostosis should be flattened and the insertion of the Achilles tendon into the heel bone should be clearly seen.

Completion of Removal of Haglund’s exostosis
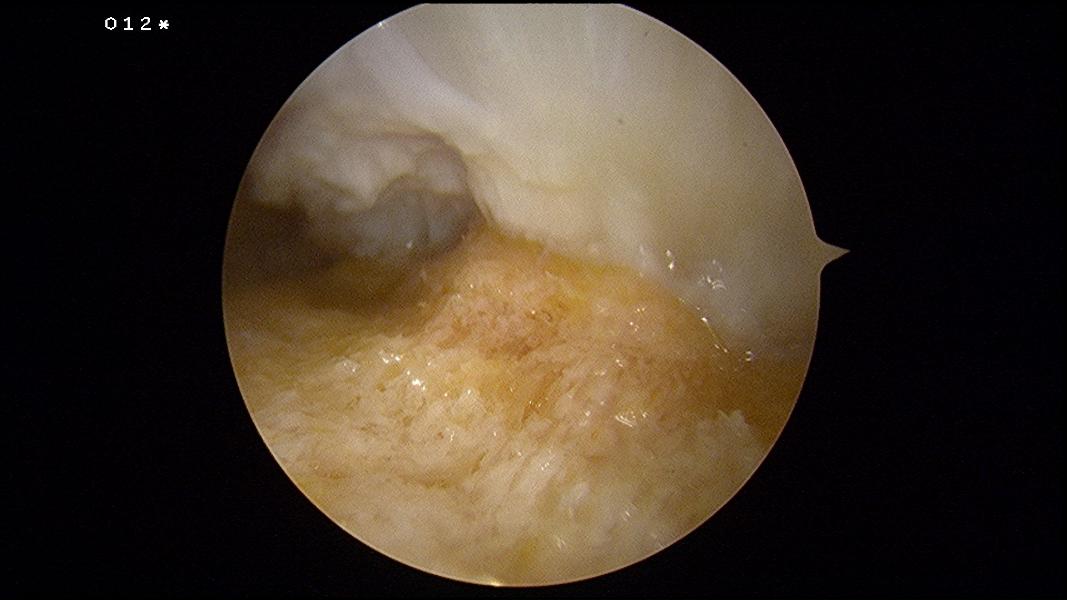
View from lateral portal showing the Achilles tendon insertion
An intra-operative fluroscopy (x-rays) to confirm complete removal of the Haglund’s protruberance:
Pre and Post Endoscopic Calcaneoplasty
This surgical scar after skin closure:

Surgical Wounds in Endoscopic Calcaneoplasty
Post-Surgical Recovery The patient is allowed to walk with the help of crutches and avoid bearing weight in his operated foot for the next 3 weeks. The operated foot should be elevated for at least 3 to 5 days. The surgical wound should heal in 14 days after surgery and the stitches are removed. The patient can start putting more weight on the operated foot from 3rd week onwards. He can resume running in 3 months’ time. The success rate of this procedure has been quoted to be 90%.
Find out more about other related foot and ankle injuries from our foot and ankle specialist in Singapore.